These two days were days filled with TONS of education and teaching us how to care for Sara once we went home.
First, we met with a dietician from the PDRC. She gave us an hour class on the basics of carb counting and figuring insulin doses. At each meal, Sara receives a dose of insulin 15 minutes before she eats. So we need to have her plate figured out so we can measure all the carbs. Thanks to apps and charts, this task is made easier. There are two formulas that mad up her meal dose. The first formula is the carbs she will be eating for that particular meal. Since her body doesn't make insulin to process her food, we have to give it to her. The second part of the dose is her correction dose. This is based off her blood sugar before her meals. This is what the two formulas look like:
Carbs in total meal ÷ (carb ratio)
(Blood Glucose - 120) ÷ (correction ratio)
(The carb ratio and correction ratio are variables based on her kilogram weight and blood glucose numbers. We can adjust the carb ratio by meal as we analyze her glucose numbers from day to day.)
Once we have those two numbers, we then have her meal dose. Currently, all her insulin doses are given by syringe or pen needles. We have to do this math EVERY meal.
We also learned about her basal insulin. This is the insulin that we use every day just to go through a day. It's the basic insulin in our body. She needs to have this injection every evening before she goes to bed. It's long term and lasts about 24 hours. This dosage is based on a standard formula using her kilogram weight. From there it can be adjusted up of down depending on how her glucose responds. We don't change this number very often. In fact, we have only changed it twice since diagnosis. Her meal dose has been change several times and can even be changed on a day-to-day or meal-to-meal basis.
After the dietician came in, the nurse from the PDRC gave her 1 hour class. This consisted of us learning how to draw insulin and administer shots. She had us practice with a pillow and a bottle of saline. The units are so small and with Sara's size, we round to the nearest 1/2 unit. When you are tired, those 1/2 units get even smaller! Once we learned, Daniel and I were now to give all her injections under the supervision of the nurses. Sara was and is so brave getting all these injections meal after meal, day after day
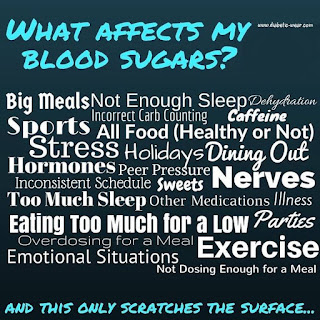
Thirdly, the family life counselor came in. Her job was to help us work through the emotional parts of the diagnosis and the financial part. She told us that grieving is a natural part of the process. Crying is a good release. Days a going to be good and days are going to be hard. No two days are going to be the same. Type 1 Diabetes is not a disease of constants. Everything affects it, everything is a variable. What works one day could send her glucose skyrocketing the next.
The financial part is a lot more difficult to navigate. Insulin is expensive. Think of a number and then you probably need to go higher, maybe even much higher. We are part of Samaritan Ministries, which we love being a part of. Unfortunately, they only cover 120 days of prescriptions. 120 days of a lifetime is not very much. So we have had to do lots of research. Thankfully, if you look hard enough, there are ways to make diabetic supplies more affordable.
As for Sara, she had several goals to obtain so she could go home. She had to have consistently lower glucose numbers, <400 preferably, and her ketones had to be moderate or small. By Friday afternoon she had accomplished both of these and had been given the green light to come home! 😀
No comments:
Post a Comment