In a previous post,I mentioned that Sara was in DKA when she was first brought to the hospital and diagnosed. Here is an article that tells the difference between ketosis, which some people use to lose weight, and ketoacidosis, which is a life threatening condition.
http://www.healthline.com/health/ketosis-vs-ketoacidosis#overview1
These are my thoughts about being the Mom of a Type 1 Diabetic and what happens in her daily life. I pray that this blog will educate others about this disease and that someday there will be a cure.
Thursday, March 30, 2017
Monday, March 27, 2017
A Day in the Life of Sara
Here is a little insight into Sara's day as a Type 1 Diabetic
7:00a Dad wakes the kids and the family gathers for family worship
7:45a Sara figures out what she wants for breakfast. We do a carb count, check her glucose, do the math and give her her first injection of the day.
8:00a Sara is usually eating breakfast. She needs to eat about 10-15 minutes after her injection. That usually gives her enough time to make whatever she has chosen to eat that day. Lately her breakfast of choice has been vanilla yogurt, granola, and scrambled eggs. Sometimes she has an english muffin with her eggs. A couple times a week she will add juice, but that really spikes her numbers before lunch and it's really not worth having to take extra insulin.
9:00a school starts. If she's not feeling well we may go lighter on the book work. The last couple of weeks she has been able to complete most of her schoolwork.
10:15a Snack time. In an ideal world, she really needs to have 2 hours between meals and snacks to have the insulin properly working. While we are at home, it is fairly easy to stick to that. Most of her snacks during school are 10g or less. We don't have to cover those 10g with insulin, so they are "free" carbs.
12:15p Lunch time is soon so Sara needs to plan her lunch. We do another carb count, check her glucose, do the math and do her second injection of the day.
12:30p Lunch. This varies from day to day. She really likes grilled ham and cheese with pineapple on the side. Sometimes Strawberries. Or maybe cucumbers with Ranch.
After lunch she likes to run around outside. We have to keep an eye on her glucose numbers. Moderate activity can cause those numbers to go down very quickly. So we have a chart that helps us keep those numbers in a healthy range. Depending on the length of activity and what her glucose is at the beginning of said activity, she needs to eat so many carbs. So before she goes out, we do another glucose check. Then when she comes back in we do another. If she is in target, we are happy. If she is high, we know that activity doesn't always mean her numbers will come down immediately. Sometimes there is a delayed reaction. So we'll test again in an hour or so. If her numbers are low, we have another chart to direct us what to do to bring her back up to target. If she is below 70 we treat with 15g of fast acting sugar like 2 packs of smarties and retest in 15-30 minutes. If she is low, but above 70, we can give her a 15g snack such as a granola bar. It doesn't need to be fast acting, but something to bring her back up to a not-so-low number. I have an alarm set for 3p so she can have a snack as needed to hold her until dinner.
5:45p Dinner will be soon. Once again we measure out her meal, carb count, check glucose, do the math and give her the 3rd injection of the day. When she is finished we begin to gather at the table. By the time we sent and pray over the food, the 15 minutes have passed and she can eat.
8:30p Time for her long-acting insulin injection. This one burns a little. A trick one of the nurse taught us is to numb the area with ice. That seems to help quite a bit. Once again we will do a glucose check. If her numbers are high we may give her 1/2 of a correction dose. if they are low, she needs to have a hard carb snack. Usually a few crackers or some nuts.
2:00a Daniel's phone alarm goes off. Upstairs we go to check her glucose again. Usually it is in a safe range and we just go back to bed. A few times it has been too high and we have had to give 1/2 a correction dose. We also have had a low we had to treat. A pack or two of Smarties (15g fast acting sugar) and sit up for about 30 minutes and then retest. Go to bed if it is ok, or give a bit more sugar if it is still low. There have been a few times when we have gotten up again at 4a to check again.
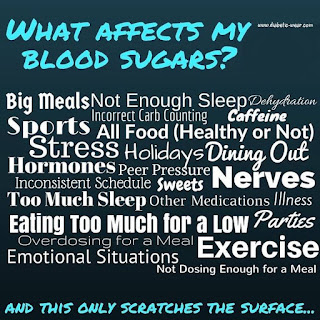
This is just a small snapshot of her day. It doesn't take into consideration the emotion, the frustration, the tiredness, days of sickness, days out of the house, fellowshipping with friends, church, or any of the other variables that life will throw at us. What works one day, does not work the next or the next. This disease doesn't sleep and neither can we. Every day we have to be on our game. No resting or taking it easy. This her life and if we are neglectful in her care, the price will be big. We aren't willing to take that risk. with our precious daughter.
1 Month Ago
1 month ago - February 28th - our lives changes forever.
The emotions associated with that day are still very fresh. The tears still well up in my eyes when I think of those first days. The first emotions were fear of the unknown and the urgency in which the ER team came around her. Usually you have to wait to be seen by the ER doctor after the nurses have been in to take vitals. Our ER doctor was waiting for us in the room with 3 nurses and 2 IVs already on the pole along with insulin to piggyback. The first things out of her mouth were notifying me that they had already called Children's to see if they had an available bed in the PICU. That will put fear into a parent.
After the initial shock wore off, my fighting spirit kicked in. I needed to be strong for Sara and advocate for her as needed. I asked question upon question and when I wasn't asking them, Daniel was. We wanted to know everything and the doctors and nurses were kind to us and tried to explain everything they were doing. We were blessed to have wonderful doctors and nurses the whole time Sara was hospitalized.
I still have times when I just break down. especially when I think of her future. While it is true that she can do and be anything she wants, there are also limitations. Yes, she can drive, but because she has a condition that can cause blackouts, she has to have a waiver from her doctor. Yes, she can get married and have children, but she can't have a home birth. This disease will affect EVERYTHING she does and every decision she makes for the rest of her life.
1 month ago - our lives changed forever.
We are stronger. I never would have thought that I could give my own daughter injections multiple times a day. I don't like needles and I hate having to hurt my daughter, even if it is just feels like a pinprick. Yet I have had to give her over 112 injections in the last month. She has pricked her own finger over 180 times in the last month. That's only in 1 month and she has a lifetime to go. We may cry lots of tears and endure heartache, but we are stronger because of it. We will not let Type 1 bring us down. We will fight and we will fight until there is a cure.
1 month ago - our lives changed forever.
Our faith is stronger. God knew from the beginning of time that our daughter was going to have this disease. He knew the day she was going to go into DKA and be hospitalized. Not one part of this was out of His control. Type 1 is making us stronger, but not because of anything we are doing. We don't have to fight this disease alone. We have days that we feel overwhelmed and feel alone, but we aren't because God is carrying us through these hard days and He will be there right beside us forever.
Articles on Type 1 Life
Here are some articles that give a little bit of insight into the life and thoughts of diabetics and their families.
Tips for Type 1 Parents
http://www.healthline.com/diabetesmine/tips-for-type1-diabetes-parents#6
"When children are first diagnosed, parents are exhausted, running off little sleep and raw emotions with no light at the end of the tunnel. They are in education overload, having to learn so many things to take care of their child and keep them alive. They frequently get no breaks because there are usually few people who can take over care for a child with diabetes. Even having a night out with a sitter is difficult."
Tips for Type 1 Parents
http://www.healthline.com/diabetesmine/tips-for-type1-diabetes-parents#6
"When children are first diagnosed, parents are exhausted, running off little sleep and raw emotions with no light at the end of the tunnel. They are in education overload, having to learn so many things to take care of their child and keep them alive. They frequently get no breaks because there are usually few people who can take over care for a child with diabetes. Even having a night out with a sitter is difficult."
What Are D-Moms made of
"D Moms are made of encyclopedias: Information? We have retained it. We are the go-to information source for our children's health. We are the experts. Yes...you can site that."
What Type 1 looks Like
"It looks like regular people living regular lives. But nothing is regular. Every moment is touched by this disease. No days off. What is eaten, what is done, where is traveled, it is all touched by blood sugars and insulin."
Sometimes vs Most of the Time
"Sometimes, I’ll look at a pile of bloody test strips on the dresser, (aftermath from a long night,) and I throw up a little in my throat. It is the grizzly reality of our life. Sometimes, there can be 20 test strips lying on the boys' dressers from the evening before and a couple checks through the night. I pick each one up to throw in the garbage. It hurts my heart as some of them stick to the dresser. Tears come as I wonder if this will always be our reality. Wondering if there will ever be a cure. The image throws me…and validates all my anger towards this disease. I think of their callused fingers and I want to roar like a mother lion that is protecting her young. Sometimes."
Type 1 Diabetes
During all our hours of education, the dietician and nurses keep reinforcing that isn't how it works. Sara can eat anything she wants, just in moderation. Low carb/high fat diets aren't good for her. She needs the carbs to fuel her cells to grow. Choosing healthy carbs over junk food is obviously much better for her and for everyone.
As we continued to attend education classes and do research on our own, we realized that Type 1 is nothing like Type 2. They shouldn't even both be referred to as diabetes.
As the picture about shows, Type 1 is an autoimmune disease. Sara's islet cells in her pancreas are being attacked by her own body causing it to not produce insulin. The only way she can get insulin is for us to inject it through syringe, pen, or pump. Because she has one autoimmune disease, she is at risk for other autoimmune diseases such a Hypothyroidism, Celiac, Rheumatoid Arthritis, and others. She will have screening for the antibodies for these diseases.
There is nothing we could have done to prevent this disease. We did mistake the early warning signs as the flu and normal childhood ailments, but we did not cause the disease. It had been dormant in her body and we're pretty sure that a virus kicked it into action. There is no cure. Essential Oils, diet, lifestyle changes, cinnamon, herbs, etc. can not cure her or even change the course of the disease. If it could, we would. Its heartbreaking watching your daughter fight this disease and know there is nothing you can do to heal her.
Sara needs to have insulin every day. Some think that insulin is a cure. It is not. Insulin to Sara means LIFE. Without it, she will get sick and die.
Type 1 diabetes is non stop. Managing Type 1 is a 24/7/365 job. There are no vacations or holidays. Diabetes does not sleep. In fact we aren't sleeping all night either. We are up at least once with her every night, checking her glucose numbers. Some think that decisions are made only at meal time. That's only a small part. Every activity requires glucose checks. Jumping on a trampoline can cause her sugars to tank. So she has to have carbs before so she doesn't go low. When she goes low, we have a protocol to follow. If she's sick, another protocol. If she's high another protocol. It takes quick reflexes to fix lows. Type 1 is a never ending thought process. I plan on putting together a post snapshotting her day.
The following is a video that tells in 1 word how people feel about Type 1 (most use more than 1 word):
HOME!!
Walking out of that hospital with Sara never felt so good. OSF has Valet parking, which is wonderful to use. Yes, you can park your own car, but when you have a baby and other things, plus everything you collect in the hospital, it's nice to have someone just pull the car up for you.
On our way home we had to stop and fill all Sara's prescriptions. Two types of insulin, syringes, ketone strips, test strips, and Glucagon. While were waiting at Walgreens, I sat and nursed Selah, while Daniel ran Sara home. Thankfully home isn't far away, as Selah had a huge blowout diaper. So around her turned to get her a new outfit and blanket. That was just the beginning of a rough evening.
Once we got home, it was getting close to dinner time. So we counted the carbs and got the supplies ready. It was like taking care of a newborn as first time parents. You are awkward, wondering if you are remembering how to do everything the way it is supposed to be done. We opened up the insulin and it didn't look correct. They had given us pen cartridges instead of vials and we didn't have a pen! Could we use a syringe on the cartridge? Then her glucose monitor said "HI". Try another one. That said "HI" too. So we made our first call to the doctor. An hour later, with a starving child and parents, we finally were able to sit down and eat. Then it was time to check ketones. They were large again. So another call to the doctor who had us gave us more instructions. Bedtime finally came and we all collapsed.
The next couple of days were all a blur of learning how to get the timing of meal prep with carb counting and then giving the insulin doing. We made it through with lots of tears, hugs, and by the grace of God.
On Sunday, Sara and Daniel stayed home from church. It felt good to do something normal. Everyone had lots of questions. My logical, non-emotional side kicked in and the technical just started flowing. Most people are familiar with Type 2 Diabetes and Type 1 is so different. I'll save that information for another post.
When I got back home, I was exhausted and Sara had her first big emotional meltdown. Her and I just had tears running down our faces. Was she ever going to be normal? Why did this happen? question after question came out. It was good for both of us to talk through everything. One thing that has been very important for Daniel and I is to keep reaffirming to her that God knew all this was going to happen before she was even created. Psalm 139 reminds us that we are fearfully and wonderfully made. God didn't make a mistake when he created her or allowed this disease to happen. We don't now why, but we do know it is for our good. Our faith sure has grown since this diagnosis.
On our way home we had to stop and fill all Sara's prescriptions. Two types of insulin, syringes, ketone strips, test strips, and Glucagon. While were waiting at Walgreens, I sat and nursed Selah, while Daniel ran Sara home. Thankfully home isn't far away, as Selah had a huge blowout diaper. So around her turned to get her a new outfit and blanket. That was just the beginning of a rough evening.
Once we got home, it was getting close to dinner time. So we counted the carbs and got the supplies ready. It was like taking care of a newborn as first time parents. You are awkward, wondering if you are remembering how to do everything the way it is supposed to be done. We opened up the insulin and it didn't look correct. They had given us pen cartridges instead of vials and we didn't have a pen! Could we use a syringe on the cartridge? Then her glucose monitor said "HI". Try another one. That said "HI" too. So we made our first call to the doctor. An hour later, with a starving child and parents, we finally were able to sit down and eat. Then it was time to check ketones. They were large again. So another call to the doctor who had us gave us more instructions. Bedtime finally came and we all collapsed.
The next couple of days were all a blur of learning how to get the timing of meal prep with carb counting and then giving the insulin doing. We made it through with lots of tears, hugs, and by the grace of God.
On Sunday, Sara and Daniel stayed home from church. It felt good to do something normal. Everyone had lots of questions. My logical, non-emotional side kicked in and the technical just started flowing. Most people are familiar with Type 2 Diabetes and Type 1 is so different. I'll save that information for another post.
When I got back home, I was exhausted and Sara had her first big emotional meltdown. Her and I just had tears running down our faces. Was she ever going to be normal? Why did this happen? question after question came out. It was good for both of us to talk through everything. One thing that has been very important for Daniel and I is to keep reaffirming to her that God knew all this was going to happen before she was even created. Psalm 139 reminds us that we are fearfully and wonderfully made. God didn't make a mistake when he created her or allowed this disease to happen. We don't now why, but we do know it is for our good. Our faith sure has grown since this diagnosis.
Day 3 & 4
DAY 3 & 4:
These two days were days filled with TONS of education and teaching us how to care for Sara once we went home.
First, we met with a dietician from the PDRC. She gave us an hour class on the basics of carb counting and figuring insulin doses. At each meal, Sara receives a dose of insulin 15 minutes before she eats. So we need to have her plate figured out so we can measure all the carbs. Thanks to apps and charts, this task is made easier. There are two formulas that mad up her meal dose. The first formula is the carbs she will be eating for that particular meal. Since her body doesn't make insulin to process her food, we have to give it to her. The second part of the dose is her correction dose. This is based off her blood sugar before her meals. This is what the two formulas look like:
These two days were days filled with TONS of education and teaching us how to care for Sara once we went home.
First, we met with a dietician from the PDRC. She gave us an hour class on the basics of carb counting and figuring insulin doses. At each meal, Sara receives a dose of insulin 15 minutes before she eats. So we need to have her plate figured out so we can measure all the carbs. Thanks to apps and charts, this task is made easier. There are two formulas that mad up her meal dose. The first formula is the carbs she will be eating for that particular meal. Since her body doesn't make insulin to process her food, we have to give it to her. The second part of the dose is her correction dose. This is based off her blood sugar before her meals. This is what the two formulas look like:
Carbs in total meal ÷ (carb ratio)
(Blood Glucose - 120) ÷ (correction ratio)
(The carb ratio and correction ratio are variables based on her kilogram weight and blood glucose numbers. We can adjust the carb ratio by meal as we analyze her glucose numbers from day to day.)
Once we have those two numbers, we then have her meal dose. Currently, all her insulin doses are given by syringe or pen needles. We have to do this math EVERY meal.
We also learned about her basal insulin. This is the insulin that we use every day just to go through a day. It's the basic insulin in our body. She needs to have this injection every evening before she goes to bed. It's long term and lasts about 24 hours. This dosage is based on a standard formula using her kilogram weight. From there it can be adjusted up of down depending on how her glucose responds. We don't change this number very often. In fact, we have only changed it twice since diagnosis. Her meal dose has been change several times and can even be changed on a day-to-day or meal-to-meal basis.
After the dietician came in, the nurse from the PDRC gave her 1 hour class. This consisted of us learning how to draw insulin and administer shots. She had us practice with a pillow and a bottle of saline. The units are so small and with Sara's size, we round to the nearest 1/2 unit. When you are tired, those 1/2 units get even smaller! Once we learned, Daniel and I were now to give all her injections under the supervision of the nurses. Sara was and is so brave getting all these injections meal after meal, day after day
Thirdly, the family life counselor came in. Her job was to help us work through the emotional parts of the diagnosis and the financial part. She told us that grieving is a natural part of the process. Crying is a good release. Days a going to be good and days are going to be hard. No two days are going to be the same. Type 1 Diabetes is not a disease of constants. Everything affects it, everything is a variable. What works one day could send her glucose skyrocketing the next.
The financial part is a lot more difficult to navigate. Insulin is expensive. Think of a number and then you probably need to go higher, maybe even much higher. We are part of Samaritan Ministries, which we love being a part of. Unfortunately, they only cover 120 days of prescriptions. 120 days of a lifetime is not very much. So we have had to do lots of research. Thankfully, if you look hard enough, there are ways to make diabetic supplies more affordable.
As for Sara, she had several goals to obtain so she could go home. She had to have consistently lower glucose numbers, <400 preferably, and her ketones had to be moderate or small. By Friday afternoon she had accomplished both of these and had been given the green light to come home! 😀
Day 2
DAY 2 :
The first morning dawned and so did the realization that our life had changed. Daniel had gone home to spend the night with the other children, to give them comfort and as much information he could, which as this point wasn't very much. While he was gone, test results began to trickle in. First, came the news that Sara had a virus. This particular virus required isolation. Isolation meant everyone who came into the room had to wear gowns, masks, and gloves. Since Selah and I were already in the room, we were exempt. However, we could not leave the room for any reason, except to leave the hospital.
When Daniel returned, in his lovely yellow gown and mask, Sara and I were watching some tv. I say she was watching, but she was so disconnected and out of it at this point, that I'm not sure she really knew what was going on. She would complain of pain in her legs, so I would massage them. The reason they were hurting so much is because she was so dehydrated, and her potassium levels were so low, they were causing her leg and stomach to cramp. This did improve over the course of her stay as she was rehydrated and began taking high doses of potassium.
My parents came to visit. Sara lit up a bit when they brought her a gift, but for the most part she just kept quiet and watched tv.
As the day continued on, various doctors, mostly residents, came and went. We were introduced to one of the doctors from the Pediatric Diabetic Resource Center (PDRC) where Sara now has her various appointments. This doctor (who will remain nameless), gave us tons of information of what was going on in Sara's body and what we would be doing going forward. His personality was a bit overwhelming and that was very frustrating. He did give us some good news. She was stable enough that they were going to move her to the Intermediate Floor. So instead of having the one-on-one care in the PICU, there would be 3 patients for every nurse.
Late afternoon they had everything ready, and we changed rooms. Sara was also allowed to finally eat something. This really made her happy and it was good to see her spirits improve with this news. After dinner, Justin, Melinda, Jaxon, Emil, Jesi, and Liam came to visit. They were all very concerned for her. She was so happy to see her nephews. Children under 18 were not allowed on the floor, but because they were family, they let the boys visit.
This night, Daniel stayed with Sara. It was hard to leave. I had been taking care of a lot of her needs. However, Selah and I needed some sleep, and that wasn't going to happen at the hospital. The kids at home were so excited to see both of us. The older girls gave Selah extra loving, while I snuggled with Jadon and Alexis.
After they all went to bed, and the house was quiet, I finally let the tears flow. I was grieving for not seeing Sara's sickness earlier, grieving for the loss of her innocence, and grieving for her future of needles, pokes, and constant monitoring. It is a hard thing to hear that your daughter will forever have this disease. It is a disease that is 24/7/365 - no holidays, no vacations, always there affecting every decision made.
The first morning dawned and so did the realization that our life had changed. Daniel had gone home to spend the night with the other children, to give them comfort and as much information he could, which as this point wasn't very much. While he was gone, test results began to trickle in. First, came the news that Sara had a virus. This particular virus required isolation. Isolation meant everyone who came into the room had to wear gowns, masks, and gloves. Since Selah and I were already in the room, we were exempt. However, we could not leave the room for any reason, except to leave the hospital.
When Daniel returned, in his lovely yellow gown and mask, Sara and I were watching some tv. I say she was watching, but she was so disconnected and out of it at this point, that I'm not sure she really knew what was going on. She would complain of pain in her legs, so I would massage them. The reason they were hurting so much is because she was so dehydrated, and her potassium levels were so low, they were causing her leg and stomach to cramp. This did improve over the course of her stay as she was rehydrated and began taking high doses of potassium.
My parents came to visit. Sara lit up a bit when they brought her a gift, but for the most part she just kept quiet and watched tv.
As the day continued on, various doctors, mostly residents, came and went. We were introduced to one of the doctors from the Pediatric Diabetic Resource Center (PDRC) where Sara now has her various appointments. This doctor (who will remain nameless), gave us tons of information of what was going on in Sara's body and what we would be doing going forward. His personality was a bit overwhelming and that was very frustrating. He did give us some good news. She was stable enough that they were going to move her to the Intermediate Floor. So instead of having the one-on-one care in the PICU, there would be 3 patients for every nurse.
Late afternoon they had everything ready, and we changed rooms. Sara was also allowed to finally eat something. This really made her happy and it was good to see her spirits improve with this news. After dinner, Justin, Melinda, Jaxon, Emil, Jesi, and Liam came to visit. They were all very concerned for her. She was so happy to see her nephews. Children under 18 were not allowed on the floor, but because they were family, they let the boys visit.
This night, Daniel stayed with Sara. It was hard to leave. I had been taking care of a lot of her needs. However, Selah and I needed some sleep, and that wasn't going to happen at the hospital. The kids at home were so excited to see both of us. The older girls gave Selah extra loving, while I snuggled with Jadon and Alexis.
After they all went to bed, and the house was quiet, I finally let the tears flow. I was grieving for not seeing Sara's sickness earlier, grieving for the loss of her innocence, and grieving for her future of needles, pokes, and constant monitoring. It is a hard thing to hear that your daughter will forever have this disease. It is a disease that is 24/7/365 - no holidays, no vacations, always there affecting every decision made.
Sunday, March 26, 2017
The Beginning - Day 1
February 28th, 2017. A day that forever changed our lives. Sara had been not feeling well for several days. Just run down, complaining of an occasional stomach ache and achy legs. I also had commented to Daniel that she looked like she had been losing weight. We chalked all that up to a virus that was going through the family and the fact she had gone through a growth spurt. On Monday, the 27th, she stayed on the couch all day. I asked Daniel if we should take her to the doctor and we agreed that if she wasn't better on Tuesday I would call. Tuesday morning, the 28th, she woke up around 6am breathing very heavy and just feeling awful. I called the doctor and they didn't have any appointments for that day. It's probably just the flu, so push fluids and call us in the morning. We gave her gatorade and tried to get her to eat. She just kept complaining, to the point of tears, that she felt awful and everything, especially her legs and stomach, hurt. We decided that a trip to Urgent Care at Pekin Hospital was in order. She could hardly walk, but we made it to the office. Once we checked in, they took us back to do vitals. As soon as the nurse did that, she immediately left the room. That made me very uneasy. She came back quickly and said, "We can't handle this, you need to go to the ER." They put her in a wheelchair and off we were to the other side of the hospital. By the time we walked into the room, there were 3 nurses and the doctor bustling around, setting up 2 IVs and taking vitals. There was such an urgency. The doctor informed me that Sara was very sick and that they had already connected OSF Children's Hospital for transport and a PICU room. At this point, I called Daniel at home. Choking back tears, I told him he needed to some immediately because Sara was so sick, and they were setting up transport to Peoria. He gathered up Selah and came to be with us. By this time, they had tested her blood glucose and it was over 500. They started insulin and were using the term diabtetes. We were in such a fog, trying to absorb everything they were trying to tell us.
While we were waiting for transport, Daniel began sending out emails and making phone calls to church and family members. We didn't know what exactly was happening or what the next hours would bring, but we did know that we needed people to pray.
After about 3 hours, we got word there was a bed for Sara and transport was ready for us. Daniel took Selah in the van and I was able to ride in the ambulance with Sara. She remembers the trip a bit, despite the fact she was fairly out of it. Once at Children's, we were taken immediately up to the PICU where 2 nurses met us. They got Sara into the bed and hooked up to the various machines getting her vitals. The PICU doctor came in and gave us the news. She was in Diabetic Ketoacidosis (DKA) (http://www.mayoclinic.org/diseases-conditions/diabetic-ketoacidosis/basics/definition/con-20026470). Basically her body was eating itself. Since he body wan't producing insulin, it couldn't use carbs for energy for her cells. So the body begins to burn fat for energy leading to weight loss. By the time we figured it all out, she probably lost 15-20 lbs in a very short period of time. They also confirmed that this all started because of Type 1 Diabetes. We knew next to nothing about this disease that was now a part of our family. Over the next few days, we would receive information left and right. For now, though, our concern was getting insulin and fluids into Sara. Tons of labs were drawn, IV bags filled, and every two hours her blood glucose checked. Bryan and Kim Evans came to the hospital to sit with us for a bit and pray with us. Our minds were still numb, so it was a blessing to have friends come and just be with us.
The hospital allowed Selah to stay with us. We were very grateful for that considering they had a flu policy in place for visitors. Having her with me, allowed me to take care of Sara without having to worry about where my baby was and how I was going to nurse her. She was such a good baby, and hardly made a peep the whole time we were there. I stayed that first night, hardly getting sleep. I wanted to know everything they were doing and why. The more information they gave me, the more I felt in control. It was a false feeling, but I couldn't lose it in front of Sara, no matter how bad my heart was breaking.
While we were waiting for transport, Daniel began sending out emails and making phone calls to church and family members. We didn't know what exactly was happening or what the next hours would bring, but we did know that we needed people to pray.
After about 3 hours, we got word there was a bed for Sara and transport was ready for us. Daniel took Selah in the van and I was able to ride in the ambulance with Sara. She remembers the trip a bit, despite the fact she was fairly out of it. Once at Children's, we were taken immediately up to the PICU where 2 nurses met us. They got Sara into the bed and hooked up to the various machines getting her vitals. The PICU doctor came in and gave us the news. She was in Diabetic Ketoacidosis (DKA) (http://www.mayoclinic.org/diseases-conditions/diabetic-ketoacidosis/basics/definition/con-20026470). Basically her body was eating itself. Since he body wan't producing insulin, it couldn't use carbs for energy for her cells. So the body begins to burn fat for energy leading to weight loss. By the time we figured it all out, she probably lost 15-20 lbs in a very short period of time. They also confirmed that this all started because of Type 1 Diabetes. We knew next to nothing about this disease that was now a part of our family. Over the next few days, we would receive information left and right. For now, though, our concern was getting insulin and fluids into Sara. Tons of labs were drawn, IV bags filled, and every two hours her blood glucose checked. Bryan and Kim Evans came to the hospital to sit with us for a bit and pray with us. Our minds were still numb, so it was a blessing to have friends come and just be with us.
The hospital allowed Selah to stay with us. We were very grateful for that considering they had a flu policy in place for visitors. Having her with me, allowed me to take care of Sara without having to worry about where my baby was and how I was going to nurse her. She was such a good baby, and hardly made a peep the whole time we were there. I stayed that first night, hardly getting sleep. I wanted to know everything they were doing and why. The more information they gave me, the more I felt in control. It was a false feeling, but I couldn't lose it in front of Sara, no matter how bad my heart was breaking.
Subscribe to:
Posts (Atom)
We Are D mamas
(Reprinted with permission) We are the D Mothers We are called D Moms. D Mamas. Even Type 3's. Sometime...
-
(Reprinted with permission) We are the D Mothers We are called D Moms. D Mamas. Even Type 3's. Sometime...
-
Having a t1d (type 1 daughter) has taught us many new things. One of these is a whole new language. Here is one of the Slang "dictionar...
-
1 month ago - February 28th - our lives changes forever. The emotions associated with that day are still very fresh. The tears still we...